Blood sugar measured by lasers
Search for a non-invasive technique progresses
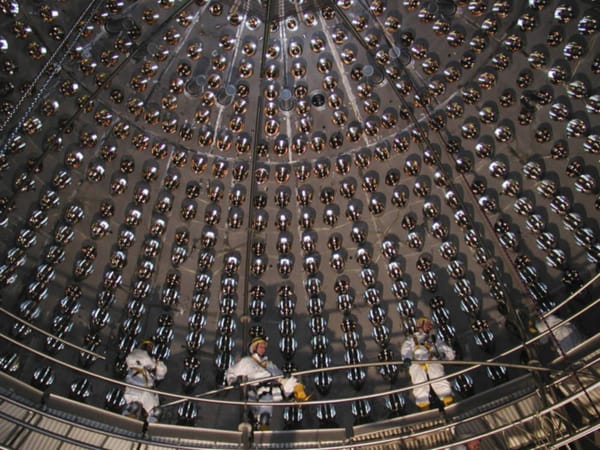
The search for a non-invasive, effective technique with which to measure the blood sugar levels of diabetes sufferers has long occupied researchers in the medicine and applied biophysics communities. For the last 20 years, research has centred on the potential use of wavelength-modulated laser radiometry – that is, shining lasers tuned to specific wavelengths at human blood samples and measuring the response.
New research by Andreas Mandelis of the University of Toronto has followed this blueprint but made some changes that may prove to be an innovative leap forward. The wavelength often used in past studies is in the near-infrared, but Mandelis and team focussed instead on differing wavelengths of mid-infrared light, utilised in two laser beams simultaneously.
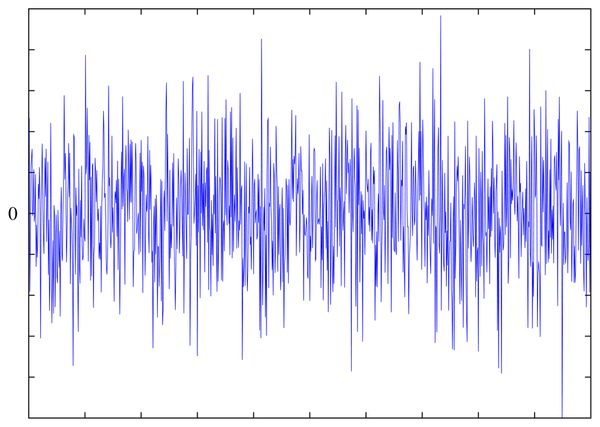
The method involved relies on the chemical bonds present in the glucose molecule. Laser light can pass harmlessly through layers of human skin and interact with molecules present within human blood plasma. As glucose molecular bonds are hit by laser light at certain frequencies they absorb energy and vibrate, thus creating a measurable response. This glucose fingerprint is, however, quite tricky to isolate due to the very nature of human blood; water is an overwhelmingly strong absorber of mid to near-infrared light, and blood is composed of approximately 92% water by volume.
However, this did not stump Mandelis and colleagues, who instead made use of this strong wavelength dependency by tuning two laser beams to very slightly different wavelengths — one that is prone to absorption by both water and glucose, and one just bywater. When both of these beams are focussed on the jumble of molecules that make up human blood, the water absorptions effectively cancel out and the returned signal is solely due to glucose absorption. This highlights the glucose levels within the blood and minimises the interference caused by water molecules.
This non-invasive and pain-free method has shown great promise in being highly sensitive to even trace amounts of glucose present in the test substance. However, there is a long way to go before the method can be considered as tried and tested; so far the procedure has only been trialled on samples of blood serum and sugar dissolved in water. Mandelis is currently working with colleagues at Toronto hospital to enable a testing programme involving human patients.
The team hope that their work may eventually lead to mass commercialisation of the technique for use in hospitals to continuously monitor diabetic patients, with the added potential for miniaturisation for use in the home.
This may be very difficult to achieve; the nature of the work involved brings many inherent restrictions such as the size and sophistication of the lasers involved, the need for personalisation to each patient before use, and inevitable price limitations.
If, however, this were possible, it may lead to a greater in-depth understanding of diabetes itself. The ability of lasers to continuously measure blood sugar levels is hugely contrasting with the current method, which can only analyse samples of blood taken at discrete time intervals.
Despite the fact that such research is as yet unproven on human patients, the method shows greater promise than comparable past studies. The frequency of research in this areareflects the importance of pioneering a successful technique in order to fully understand the disease and aid its sufferers in the future.
Mandelis and colleagues describe their research in full in an upcoming issue of Physical Review E.