Antibody treatment for cancer
There is plenty of on-going research in the field of battling cancer, whether chemically, physically or biologically. A research group from southern California is developing a new strategy on improving the transport of medicine within the patients’ body, by creating antibodies which only activate...
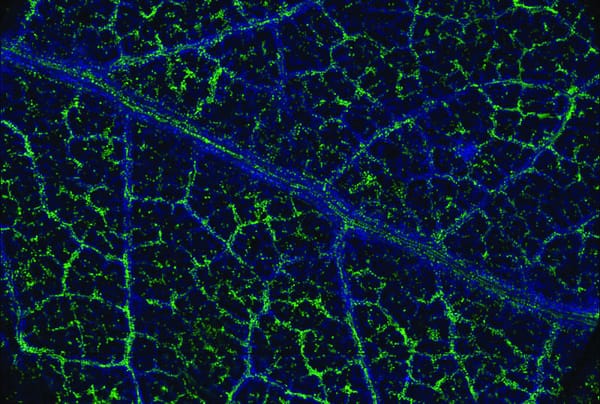
There is plenty of on-going research in the field of battling cancer, whether chemically, physically or biologically. A research group from southern California is developing a new strategy on improving the transport of medicine within the patients’ body, by creating antibodies which only activate in the presence of cancer cells. The idea of using monoclonal antibodies (antibodies cloned from a unique parent) is not a new one, and has existed for almost a century. However, due to side effects and the way certain antibodies attack the cancer cells, there has only recently been approval for their use. For example, the Cetuximab antibody releases antigens which can become toxic to skin cells in high doses, limiting the effectiveness of this treatment. Attempts to use antibody-drug conjugates have shown potential, but are still limited due to skin toxicity. However, due to healthy tissue cells expressing similar properties to the diseased cells, the antibodies are not always able to make the distinction and may target healthy tissue too. A solution was proposed by a team of researchers led by Desnoyers Luc, to mediate the toxicity of the antibodies based on the surrounding cells. While the antibodies would still have the power to knock out cancerous infections, they would only release the antigens in the presence of the intended cells. The research group developed the EGFR antibody PB1 based on the previously trialled Cetuximab and their tests have shown hopeful results. Comparing the two in mice tissues, PB1 and Cetuximab both showed close to 80% reduction in cancer cells. However, when tested in primate cells, Cetuximab caused the predicted skin toxicity, although no such observation was made in the PB1-treated bodies. Further tests were conducted at higher doses, and for longer periods, after which mild dermal toxicity was found, but at a less severe level than the Cetuximab. Analysis and research are continuing in this area, but with more hopeful results being shown, this could develop into quite a plausible method of treatment.