Epigenetics implicated in type 2 diabetes
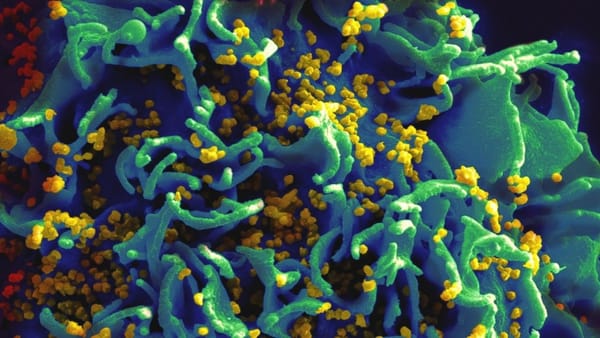
Epigenetic differences are being found in an almost-unlimited number of diseases: cancer, epilepsy, arthritis, obesity. A recent paper published in PLoS Genetics has now found that epigenetic changes may influence how susceptible one is to type 2 diabetes.

H
ow can the body change how a gene acts without changing the DNA sequence of said gene? Part of the answer lies with epigenetics: alterations to a genome that don’t happen by messing with the nucleotide sequence of DNA but by changing how the gene is expressed.
Common changes include DNA methylation, which normally suppresses gene expression, and the addition or removal of histone proteins from a gene sequence. Histones act like spools, winding up DNA so that it doesn’t take up as much space as it ultimately could.
Epigenetic differences are being found in an almost-unlimited number of diseases: cancer, epilepsy, arthritis, obesity. A recent paper published in PLoS Genetics has now found that epigenetic changes may influence how susceptible one is to type 2 diabetes.
Type 2 diabetes develops happens when your pancreas either doesn’t produce enough insulin to maintain a normal blood glucose level – called insulin deficiency – or your body is unable to use the insulin that is produced, known as insulin resistance. Insulin is responsible for the absorption of glucose from the blood, generating cellular energy.
Researchers from Lund University in Sweden compared cells that produce insulin in healthy individuals to those who suffer from type 2 diabetes. They found that over 800 genes in diabetic individuals have epigenetic changes that aren’t observed in healthy people.
102 of these epigenetic alterations were proved to cause differential gene expression in diabetic individuals. Ultimately some of the affected genes contribute to reduced insulin production, which can be one of the underlying causes of type 2 diabetes.
Type 2 diabetes is typically treated by changing one’s diet and exercising regularly, to maintain normal blood glucose levels. But as the disease cannot be cured, treatment may eventually include using medication to control blood glucose levels.
Charlotte Ling, who led the study, said, “[Our research] can help us to understand why people develop the condition. This also opens the way for the development of future drugs.”
Furthermore, the researchers found that the epigenetic changes identified in diabetic individuals “had already taken place in healthy subjects as a result of age or high BMI (body mass index)”.
This suggests that these changes may be contributing to the pathogenesis of type 2 diabetes. Future research can use this work to identify new target genes for therapy.
“Unlike genes that can’t be changed, epigenetic changes are reversible,” said Tasnim Dayeh. In fact, drugs that cause epigenetic changes have long been used in the treatment of cancer and epilepsy. This lends further support to the hope that this work could be important in developing treatment drugs.
Perhaps one day the stigma of suffering from ‘self-inflicted’ diabetes – type 2 diabetes being a condition linked to obesity and old age – will lessen, as people are able to receive the medical treatment that they deserve. We can only hope.
DOI: 10.1371/journal.pgen.1004160