Resistance is Futile: Why Antibiotic Overprescribing Remains a National and Global Problem

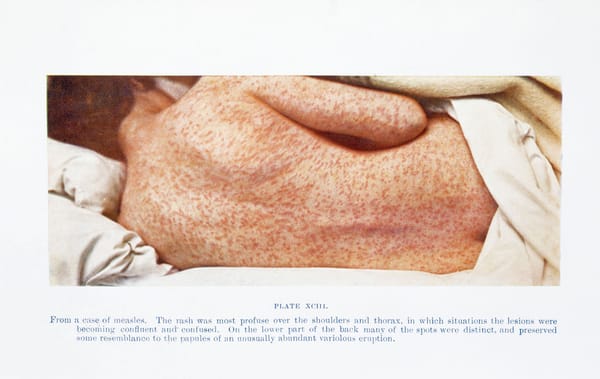
Antimicrobial resistance is a problem that we’ve known about for around 75 years now, with Alexander Fleming referring to it in his Nobel Prize speech way back in 1945. Since then the problem has become recognised internationally. It is estimated that around 700,000 people every year die from drug-resistant infections, and projections suggest that by 2050, this could rise to a disturbing 10 million deaths annually. Causes of overprescribing include expectations and demand by patients, expensive testing leading to unclear diagnoses, and excessive duration of treatment.
A recent report by NICE indicated that between 2013 and 2017, although antibiotic prescribing was reduced by 4.5%, the number of infections resistant to key antibiotics continued to rise by 35%, highlighting that antimicrobial resistance is still a major healthcare problem in the UK. It is estimated that somewhere between 9% and 23% of antibiotic prescriptions are inappropriately prescribed in English primary care. A recent study published in the BMJ compared antibiotic prescriptions in England with national guidelines and found that a substantial proportion of antibiotic courses exceeded the recommended duration of treatment.
NICE has a few recommendations in place to help combat this problem. One is its promotion of antibiotic stewardship teams, which recommend that all healthcare settings in the UK have a team of core people, including an antimicrobial pharmacist and a microbiologist, who can be consulted to provide guidance on best practice of antibiotic prescribing. NICE also has guidance on changing risk-related behaviours in the population, which focuses largely on education of the public on the dangers of overuse of antibiotics, and the dissemination of advice and resources on how to avoid the spread of infections. Furthermore, NICE is working with new funding models which aim to delink payment from the volume of antimicrobials prescribed, providing a much-needed economic incentive for the development of new antimicrobial medicines.
The national implementation of strategies to prevent antimicrobial misuse is a small step toward tackling this global problem. The widespread use of antimicrobials both in medicine and the veterinary/agriculture industries is leading to a high selective pressure which creates dangerous strains of resistant microbes, at a rate that cannot be matched by research and development into new antimicrobial medicines.