Could 'The Last of Us' really happen? An interview with a fungal expert
Science writer Sam Lovatt sits down with Matthew Fisher, Professor of Fungal Disease, to discuss the hit show and the effect of fungi on the world

In 1692 Massachusetts, several young girls became suddenly ill with bouts of unnerving symptoms, including temporary blindness, skin lesions, and hallucinations. A local doctor, unable to think of a medical reason for such afflictions, diagnosed the girls with ‘bewitchment’, a proclamation that led to the mass hysteria and mob behaviour known today as the Salem Witch Trials. As the field of medicine has advanced, scholars have sought a more robust explanation for the girls’ symptoms. One more likely than ‘bewitchment’ is ergot poisoning, caused by the ingestion of by-products of the fungus Claviceps purpurea, wellsuited for colonising moist rye crop. People who ingest rye grains infected with C. purpurea may be consuming dangerous quantities of lysergic acid, an LSD precursor that can wreak havoc on the nervous system. People suffering from ergot poisoning may appear hysterical and report crawling sensations across the skin as well as hallucinations. Continued exposure causes ergotism — also called St Anthony’s Fire — so named for the intense burning pain it causes in the extremities, ultimately leading to gangrene as blood supply is consistently cut off.
The damage caused by C. purpurea is just one of many excruciating, fascinating examples of fungal infection and toxicity that Matthew Fisher, Professor of Fungal Epidemiology at Imperial College, gives me as we sit down to talk about HBO’s new hit series The Last of Us (TLOU), and fungal pathologies in general. My idea to interview a fungus expert in the wake of TLOU’s release was not as original as I had hoped, I quickly learned. The day prior, Mat had done an interview for American broadcaster CNN on the same topic, as one of a relatively small network of fungus experts who have recently found themselves inundated with public interest (Mat pronounces it ‘fun-ji’ rather than ‘fun-guy’, if any pedants were wondering). While media requests no doubt take their toll, the attention is an overall good thing for the field; fungal diseases are largely overlooked by the public as a major health concern, even though fungal infections cause around 1.6 million deaths per year, more than those caused by HIV and malaria combined. Fungus research receives only 5% of the funding that the ‘sexier’ fields such as bacterial antimicrobial resistance, malaria, and others receive. This lack of attention leads to deaths that would be avoidable if medics were trained to spot fungal infections as well as bacterial ones; fungal meningitis treated with antibiotics will continue to damage its host unscathed.
The scope of fungal infections, even in the developed world, is astounding. Professor Fisher tells me that as many as 30% of ICU patients whose lungs were badly damaged by COVID-19 also went on to be infected by Aspergillus — a common mould present in almost every breath we take, but which is normally shut down by our immune system even before we know it’s there. For this same reason, abnormal fungal infections in the lungs of gay men were one of the first signs that the HIV/AIDS epidemic was taking hold during the ‘80s. Things are likely to get worse. Obesity rates are soaring across the world, particularly in the West, where an abundance of fatty and sugary foods lead to weight gain and increased risk of diabetes. Fungi thrive in sugary environments, and the saccharine blood of a diabetic is an optimal environment for some fungal pathogens once they enter the bloodstream. Steroids prescribed to treat severe SARS-CoV-2 infections down-regulate macrophage activity, opening the doors for fungi to slip in.
After spending far longer than planned jumping from one astounding pathogen to another (I did suggest that Mat write a popular science book on the subject, but he valiantly said he was too busy with his research) we get to the meat of why we’re doing this interview. Could a pandemic such as the one seen in The Last of Us, caused by a brain-controlling fungus, actually happen? No, is the short answer. “Fungi such as Cordyceps, the infective agent in The Last of Us spend millennia evolving to thoroughly infect and control specific species of insect. They can’t even jump from one type of ant to another. The odds of such a specific infective agent adapting to infect humans are vanishingly small, as everything the fungus uses to infect that one insect is exquisitely honed to its body. That being said, there is an analogy to be drawn with Toxoplasma gondii [a malaria-like pathogen that infects mice, causing them to behave erratically and present themselves to cats to be eaten]. T. gondii has a lifecycle that requires it be eaten by a cat, but can also infect humans, which are almost never preyed upon. Infected humans also undergo behavioural manipulation, but much more bluntly, where they essentially are just more likely to partake in risky behaviour. It’s possible that a similar jump could be made by a fungus, but it would almost certainly just result in behavioural changes and would not be transmissible to other humans once in an initial host. This would essentially leave it with a similar effect to C. purpurea. We’ve not seen this sort of expert behavioural manipulation infection spill over from insects into other animals before.”
The opening scene of the series is of a talk-show host interviewing a scientist, Dr Neuman, who paints an exceptionally bleak picture of what a fungal pandemic would look like, saying that there is no treatment and no cure. Conversely, Fisher’s most recent work has been on the spread of drug resistance in fungi. How can there be drug resistance if no drugs exist?
“Dr Neuman is partially right. He was speaking half a century ago when antifungal drugs had not been developed and there was no effective way of treating an invasive fungal infection, and today it is still very difficult. Fungi are a sister kingdom to animals, and drugs that harm fungi often also cause damage to human cells. Anti-fungal dosage has to be very specific and most act just to limit fungal growth rather than actually killing the cells. Once a fungus colonises a bodily compartment , which might be totally obscure, it can be very hard to actually deliver the anti-fungal to the correct area.”
Dr Neuman is partially right. He was speaking half a century ago when antifungal drugs had not been developed and there was no effective way of treating an invasive fungal infection, and today it is still very difficult.
Professor Fisher started his academic career as a zoologist, studying at Edinburgh University whilst focused on parasitology. The realisation that most parasitologists spend their careers studying, in his words, animal shit, led to a change of heart and a move to postdoc work in a lab researching the valley fever fungus at University of California, Berkeley. Now, having been at Imperial for 18 years, his office is on the 11th floor of the Sir Michael Uren building at the White City campus, which has one of the most astounding panoramic views of London I’ve ever seen. Stepping into his office I am bombarded by frogs. No real ones, as far as I could see, but artwork of a frog sitting next to some mushrooms flank framed copies of the prestigious scientific journals Science and Nature, displaying amphibians on their front covers in reference to Mat’s work on fungal epidemics that have devastated global frog populations. Why do amphibians get such a hard time from fungi?
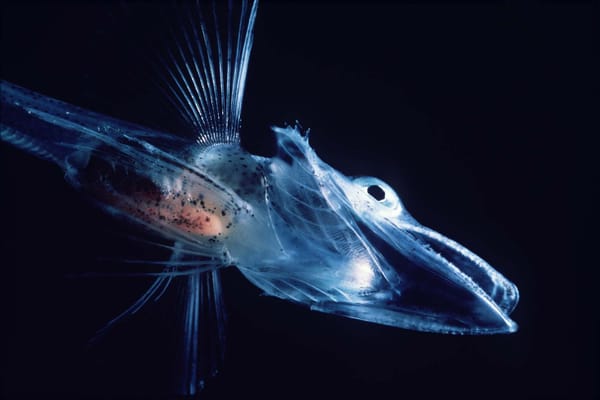
“Amphibians were the first things on four legs to leave the oceans and come into contact with the fungi that already existed on the land, and their skin is a two-way exchange that provides a perfect entry point for fungi. They had to evolve defences against invaders immediately and today’s amphibians produce an amazing array of antimicrobials from bodily glands. They are actually very resistant to fungal infections, so it was quite shocking for the scientific community to see, around the middle of the 20th century, swathes of amphibians dying across the world as a result of a fungal infection. The culprit, a chytrid fungus, was spread partly as a result of human globalisation exposing the fungus to amphibian populations that hadn’t seen it before, and is the most destructive infectious disease ever in terms of damage to biodiversity, including all viruses and bacteria. In Asia, this fungus has evolved alongside native amphibians and doesn’t cause them any harm, but other populations are defenceless. If you go to the neotropics now you will hardly hear a frog calling, as a result of this infection.”
Some viruses, such as SARS-CoV-2, can cause infection through as few as one virus particle entering the body. This is almost always not the case with fungi; a significant dose is normally required for an infection to take root, and very large doses of even the most commonplace fungus that one would find in a garden compost bin can cause a fatal infection in a healthy human. “Dosage is hugely important. Macrophages, immune cells that normally swallow anything unusual they come across in the blood, are the first line of defence against fungal invaders. If the dose is high enough to overwhelm the macrophages present in your blood, an infection can get a foothold in your body. Some fungi also have the ability to manipulate macrophages and survive even after they’ve been swallowed, which turns the macrophage from a defensive player to a vehicle that traffics the fungus around the body. We think this might be because macrophages are a lot like amoeba, single celled organisms that prey on fungi in the wild, which fungi have evolved defences against.”
There is still some reason for positivity. The World Health Organization recently released its first fungal priority pathogen list, signalling to the medical research community that fungi are a force to be reckoned with. The first ever fungal vaccine has recently shown promising results in preclinical trials, targeting the three most common human fungal pathogens all at once.
The best option is always to not open Pandora's box of pathogens in the first place.
“These advances are promising, but the best option is always to not open Pandora's box of pathogens in the first place. History shows us that we have terrible global biosecurity, and improving this through screening for fungal pathogens and reducing contamination where possible keeps the risk of new pathogens emerging as low as possible. If there’s one thing I could bring to the public’s attention it would be that we really don’t know the ecosystem-level effects of spraying fungicides in the quantities that we do today. We’re starting to see the inklings of consequences in global ecosystems, and I don’t know where that’s going to end up but it’s not going to be good”.