Curing The Incurable: Why RNA May Be The Answer To Solving Genetic Disease
RNA, despite being known primarily for its role in protein synthesis, is a particularly effective gene therapeutic.

Genetically driven diseases emcompass a wide variety of illnesses and, in addition to genetic disorders, include some of the world’s most lethal killers, such as diabetes or cancer. These occur when a specific region of DNA is deleted, replicated, or exchanged, leading to mutations and faulty protein production. While these mutations are frequently inherited, they can also arise spontaneously later in life, such as in most types of cancer.
Advanced therapies, including gene therapies, aim to treat or prevent genetic diseases by addressing the underlying cause: faulty DNA code. For example, gene-based therapeutics can be introduced to inactivate or ‘silence’ faulty genes, or conversely to stimulate expression of correctly functioning ones to amplify their effect. Genes can also be modified or reprogrammed, either within the patient or in vitro, to provide correctly functioning proteins. The type of appropriate therapy will depend on the individual’s genetic composition and stage at which the genetic mutation occurs, and so is highly tailored to the patient. This illustrates the concept of personalised medicine - and signals a move away from the current, more generalised, medication approach.
RNA, despite being known primarily for its role in protein synthesis, is a particularly effective gene therapeutic. Due to its diverse biological functions, if engineered correctly, it encounters significantly less obstacles when entering our cells than synthetic drugs, and has less potential for toxic side-effects than, for example, viral vectors, which can risk unwanted mutations or immune hyper-reactions. Moreover, small nucleotide changes can be easily made to adjust the RNA’s functions within the cell, simultaneously achieving a more targeted and versatile mode of action than currently used treatments. It is also increasingly easier and cost-effective to manufacture than more complicated alternatives, such as immunotherapies.
A currently popular method which employs RNA is CRISPR-Cas9, where a pre-designed targeting guide RNA (gRNA) sequence is embedded within a longer RNA strand (yes, it is this mechanism which was the basis of this year’s Nobel Prize in Chemistry!). The CRISPR-Cas9 complex, guided by the gRNA, binds to a specific DNA sequence inside the patient’s cells, and the Cas 9 enzyme acts to cut the DNA at this location. This triggers the cell to recognise that DNA damage has occurred and activate its own repair machinery to add, replace, or delete a gene fragment - such as a piece of faulty genetic code. CRISPR itself is extremely versatile and has high potential for a plethora of genetic diseases, but it is not yet widespread for human use, as off-target effects and other limitations are still being eliminated via early-stage studies. However, one current experimental focus is attempting to cure Huntington’s disease in humans, a genetic disease classified by additional, repeated segments of genetic code that cause deformation of the subsequently generated protein, which disrupts the functioning of neuron cells. Use of CRISPR gene editing tools aim to remove the surplus repeats to prevent escalation of the disease.
Although the most high-profile, RNA gene therapies are not limited to CRISPR tools. A type of RNA known as mRNA (messenger RNA) can be used, focusing on replacing a patient’s faulty mRNA, such as in cystic fibrosis, a disease that occurs as a result of the mutated CFTR protein. mRNA is a form of RNA which acts as the connection between protein expression and raw DNA code, and so delivering healthy mRNA to the patient could correct an underlying genetic disorder. Candidate drugs of this type involving inhalation of nanoparticles containing healthy mRNA to help replace the faulty CFTR protein are currently being developed by TranslateBio and Moderna Therapeutics, among others.
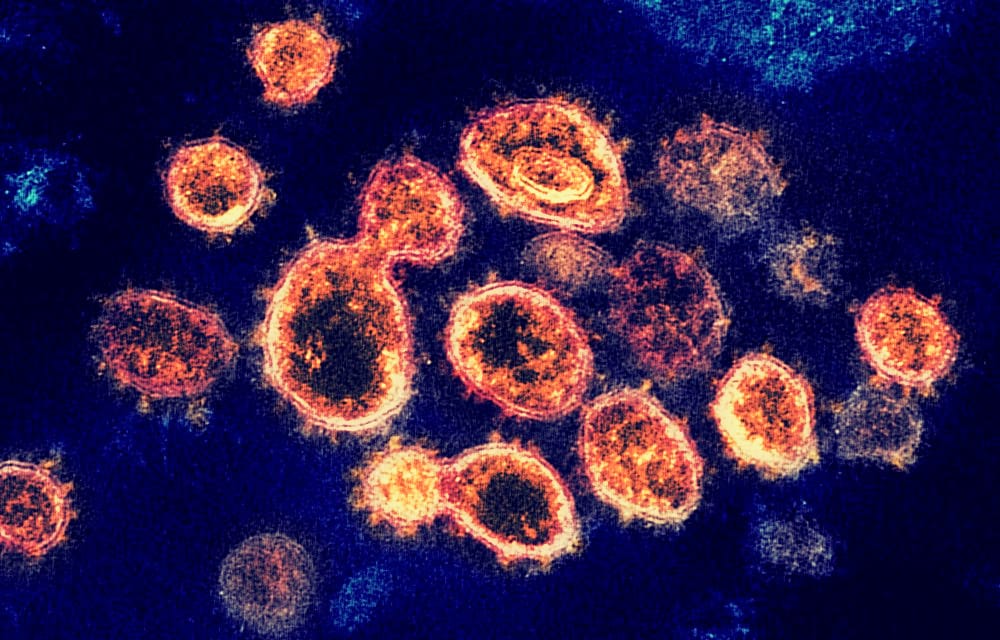
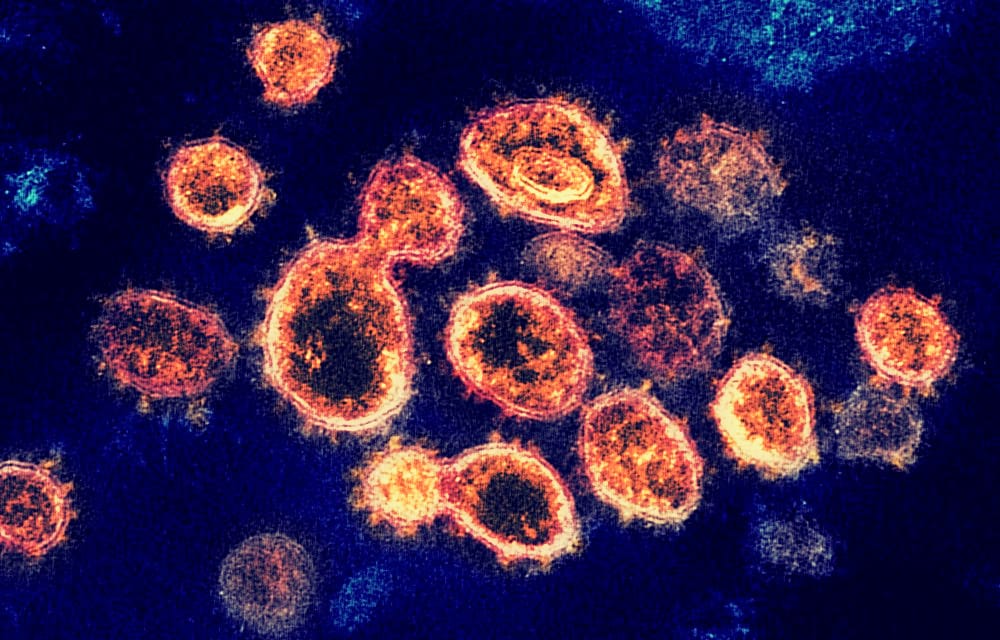
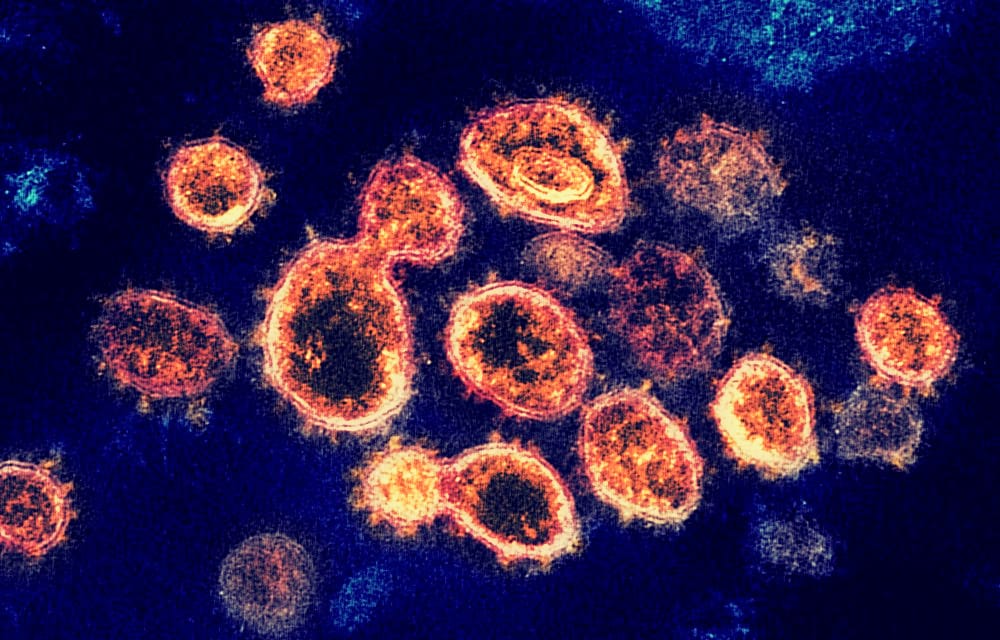
mRNA can also be used to develop vaccines; one of the leading vaccines being developed against COVID-19 is of this type and is being developed by Moderna Therapeutics. Injected mRNA can be translated into protein by our own cell machinery to stimulate the immune system, to produce a specific response against a pathogen such against the flu, Zika or rabies viruses. Specific cancer biomarkers, called neoepitopes, can also be targeted using mRNA, such as for melanoma treatment.
Finally, an RNA therapy focused on degrading faulty proteins, termed antisense therapy, is on the rise, and is currently more prominent than mRNA due to its ease of manufacture. This primarily uses a type of RNA known as interfering RNA (RNAi, or siRNA - short interfering RNA), and was the basis of the 2006 Nobel Prize in Physiology/Medicine. These short RNAs carry instructions for the cell to destroy particular malfunctioning mRNAs within itself. Again, this is gaining traction with therapies to treat haemophilia and improve kidney transplant outcomes, which are already being used, while multiple others are in clinical trials. In 2018, Alnylam Pharmaceuticals launched the first approved siRNA drug to treat a rare degenerative disorder called hereditary ATTR amyloidosis. Their drug, patisiran, is either injected or administered intravenously, and exhibits its effects in the liver; as do most candidate drugs at this point in time. Since then, however, only one other siRNA drug has been approved; but several others are showing promise in late-stage clinical trials.
RNA-based therapies hold immense potential, but the answer to the key limitation - the lack of efficient drug delivery systems which can target organs other than the liver - is the primary focus in the field. With further research and investment into the sector, RNA-based therapies appear to be the basis of the next pharmaceutical revolution, and a solid step towards curing what was once thought to be the incurable.