Exploring CRISPR-Cas9’s breakthrough genetic therapy
Felix interviews Imperial PhD student, Quentin Smith, on CRISPR-Cas9’s therapeutic potential and the significance of Casgevy approval.
In November 2023, the UK Medicines and Health Products Regulatory Agency (MHRA) became the first regulatory body in the world to grant approval to the CRISPR-Cas9 based drug Casgevy in the fight against sickle cell anaemia and β-thalassemia. This was the first drug based on CRISPR technology to be licensed for use in humans. In Felix issue 1844 on 1st March 2024, we covered Casgevy and the promise it poses.
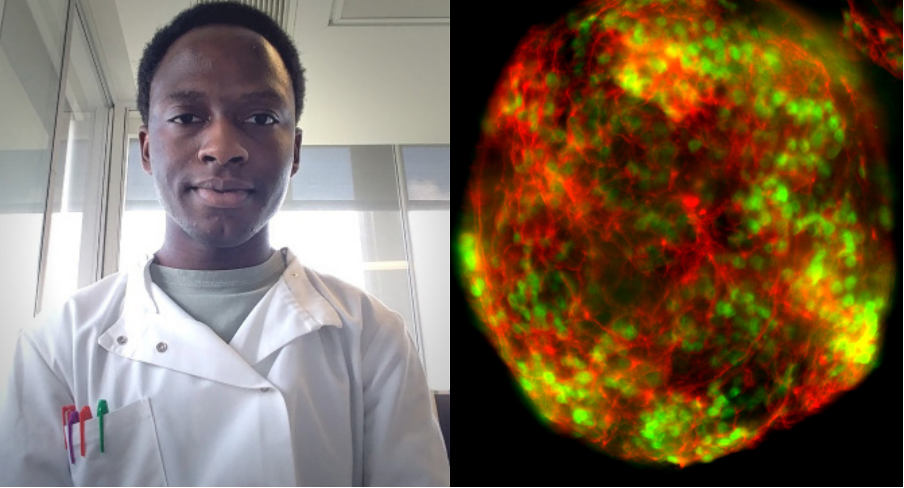
This week Felix sat down with Quentin Smith, a final year PhD student at Imperial working in Prof. David Rueda’s lab at the MRC Laboratory of Medical Sciences (LMS). Quentin’s research aims to understand genetic engineering technologies in greater detail and their implications in health and disease.
His research focuses on CRISPR-Cas9 and how it discriminates between on and off-targets.
Ever since it was engineered in 2012 by Jennifer Doudna and Emmanualle Charpentier, whose work earned them the 2020 Nobel Prize, Cas9 has always offered great promise in genome editing and the potential to cure genetic diseases. However, up until now, using CRIPSR-Cas9 in medicines has been too dangerous because it often causes off-target effects, where Cas9 binds and cuts DNA elsewhere than the desired locus. This undesirable cleavage can cause mutations and diseases worse than the original condition being treated.
Quentin Smith told Felix that his research “elucidates the molecular basis of why this occurs and provides rational on how to generate high-fidelity variants that mitigate this.”
Cas9 poses great promise in genome editing and curing genetic diseases.
Researchers not involved with the study have raised concerns that the trial of only 29 people, was not large enough to justify the licensing of the new technology. Smith, however, explained that “the amount of people who were treated and free from severe pain was quite stark - in the upper 90 percent range, which is rare to see and may have led to the approval being granted.”
Sickle cell and β-thalassemia are inherited blood disorders. Persons affected with these disorders produce little to no haemoglobin, a part of the blood that carries oxygen around the body.
Casegevy is a medicine proposed to treat blood disorders in the body. It works by reducing the number of sickle cells in the body to a negligible amount.
The drug itself is an ex-vivo treatment that uses CRISPR-Cas9. Clinicians extract stem cells from sufferers of sickle cell anaemia and β-thalassemia. These stem cells are then cultured and transfected with Cas9 that targets the BC11A gene that codes for foetal haemoglobin. These cells are then reintroduced into the patient’s body through intravenous infusion to allow them to grow and differentiate and express the corrected gene. Going slightly more into the nuances of the therapy, Quentin explained that the logic behind the genetic edits being made only to a few cells that are reintroduced and not to all cells present.
“The idea is that the transfected cells proliferate and divide and outlast the diseased cells, gradually replacing them.”
An important point to note in the approval of this drug, barring the fact that it is the first of its kind, is the data on which it was approved. Despite clinical trials having a high success rate, it has only ever been performed on less than 50 people. Many deem this to be insufficient and question whether it should have been granted approval on the basis of such a small study. Quentin commented that, “I agree that the numbers are quite low for clinical trials. I believe Casgevy is in trial phase three, which means they should have anywhere between 300-3000 people according to the Food and Drug Administration (FDA)”. Erring on the side of caution, he also noted that the clinical trials described patients being “free from severe pain”, which is quite vague. Perhaps a better definition of what severe pain symptoms are would be beneficial in addition to the empirical data the regulatory body requires.
Many scientists have warned of the ill effects of unwanted genetic mutations caused by CRIPSR based therapies. Based on his research, Quentin believes the benefits of using genetic engineering techniques do outweigh the risks. “This therapy allows the ability for you to cure many common and very rare genetic diseases.”
To take this to the next level, there has to be a lot of work to create high-fidelity Cas9 variants to reduce off target effects.
The main downside of Casgevy are the off-target unwanted genetic mutations it may cause. Quentin comments, “these clinical trials from Casgevy and others haven’t published any note on sequencing or characterisation of these off-target effects. But we know from other studies, including ours, that these o -target effects occur genome-wide, and there’s been lots of development in detections of these off-target effects”.
I agree the numbers are quite low for clinical trials. They should have anywhere between 300 - 3000 people according to the FDA
There are many different sequencing pipelines that can characterise off-target effects that don’t happen often. There is major work underway to nail down these off-target effects and mitigate their effects. While they remain a large downside of the treatment, major work is underway to reduce their effects.
“There should be a bit of a push in order to create a high-fidelity variant of Cas9. In order to take this to the next level, there has to be a lot of work to create high-fidelity Cas9 variants to reduce these off target effects and then we can go with ease into treating genetic diseases without having so much to worry about.”
“There's a bit of work on high-fidelity variance and typically the rationale behind that is through structural biology. Scientists have taken cryo-EM and X-ray crystallography structures of these Cas9 and CRISPR effectors in the presence of DNA which have on and off targets. They rationally design and create mutations between these proteins to create new high-fidelity variants which exhibit less off target effects to the ones that they observe with the wild type variants.”
“This is the main way in which they create high-fidelity variance, but there are other ways as well. You can use directed evolution, where you evolve higher fidelity variance of Cas9 using the screening assay. This is another way in which they have created high-fidelity variance. Sniper-Cas9, a high-fidelity variant of Cas9, was created using an E. coli-based directed evolution method. So, it's mainly through structural biology or directed evolution methods.”
“There's numerous of them [high-fidelity variants] available, but they still don't mitigate off-target effects enough. In order to take this to the next level, there has to be a lot of work to create high Fidelity Cas9 variants to reduce these off target effects and then we can go with ease into treating genetic disease, without having so much worry in generating more mutations or bad effects that could easily be overlooked.”
As Quentin makes very clear, therapies such as Casgevy hold great promise, and the work on mitigating any ill effects these therapies may cause means that the road looks only smooth from here on.