KCL to begin puberty blockers trial in January
The trial is steeped in controversy and surrounded by international debate on the benefits and risks of using puberty suppressing hormones.
A new clinical trial on the use of puberty-blocking drugs in children experiencing gender dysphoria is set to begin in January 2026 at King’s College London, following a ban on puberty blockers for under-18s in December 2024.
Puberty blockers can be used to treat gender incongruence, where someone’s identity doesn’t match sex registered at birth, and gender dysphoria, which is when this causes significant distress.
The clinical trial, called Puberty Suppression and Transitional Healthcare with Adaptive Youth Services (PATHWAYS), will assess puberty suppression. It runs alongside PATHWAYS CONNECT, which is an observational study that looks at brain health in those who are and aren’t taking puberty suppressing hormones.
The PATHWAYS trial will study the impact of the drugs on physical, social, and emotional wellbeing in under-16s who are currently accessing gender services and have a diagnosis of gender incongruence. It involves strict criteria and intensive medical and psychological screening before starting puberty-blocking drugs.
“We are looking very much at the balance between, possibly, benefits for mental health and quality of life, and any possible risks or harms,” explained Professor of Child and Adolescent Psychiatry Emily Simonoff, who is leading the PATHWAYS project.
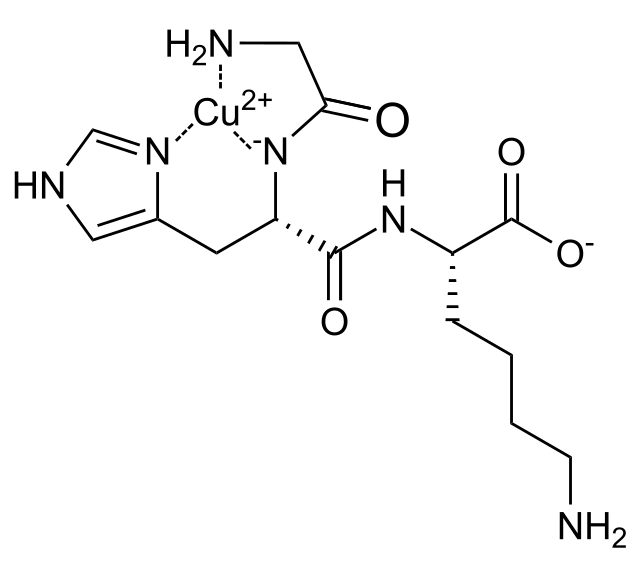
Gonadotropin-release hormone (GnRH) analogues
Puberty blockers or puberty suppressing hormones are used to delay the onset of puberty by blocking the body from producing sex hormones, such as estrogen and testosterone. The most common form of puberty blockers is known as gonadotropin-release hormone (GnRH) analogues.
Gonadotropin-releasing hormone (GnRH) is hormone produced in the hypothalamus that regulates the release of sex hormones (NIH). Many GnRH analogues are GnRH agonists, meaning they behave in a similar way to the body’s endogenous GnRH. However, GnRH analogues are more potent than native GnRH (NIH).
When a patient is given a GnRH analogue, it causes a temporary increase in sex hormone release. However, continued administration of GnRH analogues initiates a negative feedback loop, resulting in a decrease in sex hormone production. GnRH analogues do not cause a permanent change; rather, they pause puberty until the patient stops taking the medication.
GnRH analogues can be used to treat a variety of conditions, such as gender dysphoria, endometriosis, and early onset puberty (NIH).
When GnRH are used to treat gender dysphoria, they can improve mental well-being, ease depression and anxiety, and ease the thoughts or actions of self-harm, according to the Mayo Clinic. Possible side effects may include weight gain, hot flashes, headaches, and mood changes, as well as long-term effects on fertility, bone growth and density.
Previous bans on puberty blockers
A few days prior to the announcement of the PATHWAYS trial, New Zealand announced a ban on new puberty blocker prescriptions for young transgender people, which takes effect from 19 December.
A similar ban was first introduced in the UK in May 2024, following the publication of the Cass Review that April. The Cass Review, led by Dr. Hillary Cass, was commissioned by NHS England to make recommendations on how to improve the NHS’s gender identity services. The Cass Review cautioned against the use of puberty blockers, citing insufficient evidence of long-term effects on young people, but recommended establishing a puberty blocker trial.
“My review uncovered a very weak evidence base for benefits from the use of puberty blockers for children and young people with gender dysphoria,” said Cass.
The Cass Review’s methodology has been criticized. The so-called “Yale Report” - officially, it’s called “An Evidence-Based Critique of the Cass Review” - said the Cass Review “repeatedly misuses data and violates its own evidentiary standards by resting many conclusions on speculation.” The authors further added that the Review “repeats spurious, debunked claims about transgender identity and gender dysphoria.”
Ultimately, the Cass review recommended a clinical trial to make sense of the conflicting evidence. A similar sentiment was echoed by Imperial’s Professor of Reproductive Endocrinology and Andrology Channa Jayasena.
“The only way to resolve this debate is through a properly conducted randomized clinical trial - a compromise for both sides, but one that will ultimately yield the best available evidence,” Jayasena told Felix. “I hope that completion of this trial will help clarify how best to support children in this difficult situation and enable them to functional optimally in society.”
Criticisms of the PATHWAYS trial
The PATHWAYS trial is not without criticism. The government’s ban on puberty blockers was unsuccessfully challenged in the High Court in July 2024, and this trial may also end up in the High Court, according to the Economist.
One criticism is that the trial is badly designed, as it will have no placebo group. (However, having a placebo group would be highly unethical.) Every participant will receive puberty suppressing hormones, either immediately or after a year, alongside psychological therapies.
There are worries about unpredictable side effects. Animal studies have pointed to possible long-term cognitive impairments, but many questions remain.
Critics suggest other ways to collect this data, such as using health records of individuals who have already received puberty blockers.
Supporters, including Health Secretary Wes Streeting, who originally announced the ban and whose own opinion on the matter has now made a sharp U-turn, say the trial is vital.
“All young people should have access to the very best medical care, guided by evidence, and delivered by qualified experts and clinicians,” said a spokesperson for Stonewall, a UK-based LGBTQ+ rights charity, in response to the ban on puberty blockers last year. “We urge the Government and policymakers to invest in delivering excellent healthcare for trans young people and to make sure the voices of trans young people and their families are its core.”
The upcoming trial focuses a societal issue on the underlying scientific evidence
The administration or prohibition of puberty blockers is a contentious issue.
The U.S. Department of Health and Human services released a report heavily criticizing puberty blockers on November 19. The American Psychological Association pushed back, arguing the report was not sufficiently supported by scientific research, and other critics said the “peer-reviewers” have previously spoken out against gender-affirming care.
A 2017 Cornell literature review found that “gender transition, including medical treatments such as hormone therapy and surgeries, improves the overall well-being of transgender individuals.” The review also noted that research in the field is limited by historical stigma and more research is needed.
“Clinical care should always be underpinned by robust evidence, and this study will help provide a better understanding of how to treat and care for young people with gender incongruence,” said Simonoff, the trial’s lead. “We know there are ongoing societal discussions about gender transition, but this research is focused solely on informing and improving healthcare by better understanding how to support the physical and mental health of young people with gender incongruence.”