The burden of antibiotic resistance
New study finds that antibiotic resistance claimed over 1.2 million lives across the world in 2019 alone

Antimicrobial resistance (AMR) is a major threat to health worldwide, claiming over 1.2 million lives in 2019 alone. According to a new study published in The Lancet, AMR has caused more deaths than either HIV/AIDS or malaria. This makes it one of the top 10 global threats facing humanity, according to the World Health Organization.
What is antimicrobial resistance?
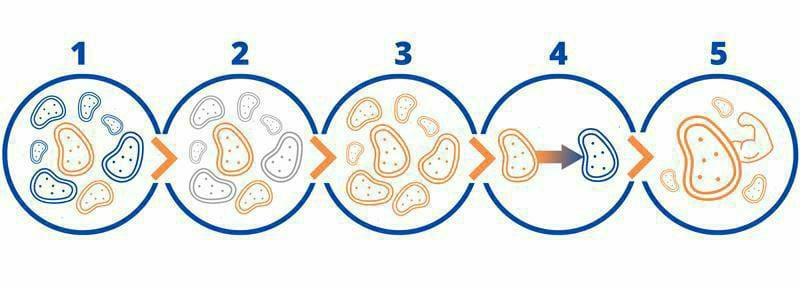
AMR happens when microorganisms (such as bacteria, viruses, parasites, and fungi) become resistant to treatments, making them unresponsive to medicine and thus making infections much harder to treat. Resistance to antimicrobials (antibiotics, antivirals, antiparasitics, and antifungals) renders these treatments ineffective against infection. Over time, this becomes increasingly dangerous as resistant microorganisms continue to grow, increasing the risk of spread, severe disease, and death as certain illnesses become untreatable. Although this process occurs naturally (microorganisms mutate naturally and are able to avoid being cleared by selective pressures such as antibiotics), it has been severely sped up by the overuse of antibiotics in humans. Over-prescription and overuse of antibiotic drugs accelerate the development of resistance by exposing microorganisms to antibiotics (see diagram). Those that have adapted will survive and continue to multiply, while those that have not adapted will die. The result is that the surviving microorganisms contain resistance traits within their DNA, which makes them resistant to certain antibiotics. Furthermore, this resistance can be spread to other microorganisms that have not been exposed to antibiotics. When microorganisms combine resistance to multiple antibiotics, they can become untreatable. Microorganisms that have become resistant to most of the commonly used medications are termed ‘superbugs’.
A global analysis of antimicrobial resistance
The first comprehensive study analyzing the impact of AMR worldwide has now been published in The Lancet, estimating that AMR-infections have led to 4.95 million deaths. Researchers have analysed data on 471 million individuals across 204 countries, using statistical modelling to estimate the effect of AMR across the world.
Here, they confirmed that AMR is now a leading cause of death worldwide, with the most deaths occurring in low- and middle-income countries. Despite this, higher income countries were also shown to have dangerously high levels of AMR. Deaths directly attributable to AMR were estimated to be highest in western Sub-Saharan Africa (27 deaths per 100,000 people) and South Asia (22 per 100,000), and lowest in Australasia (6.5 per 100,000). This study highlighted the varying impact of pathogens across the world. Whereas AMR in Sub-Saharan Africa was mostly caused by K. pneumonia (20% of deaths) or S. pneumoniae (16%), in higher income countries it was primarily attributed to S. aureus (26%) or E. coli (23%).
The six leading pathogens associated with AMR (Escherichia coli, followed by Staphylococcus aureus, Klebsiella pneumoniae, Streptococcus pneumoniae, Acinetobacter baumannii, and Pseudomonas aeruginosa) were found to be directly responsible for 929,000 deaths, and associated with 3.57 million deaths in 2019. Notably, one singly pathogen-drug combination directly caused over 100,000 deaths in 2019 alone – methicillin-resistance S. aureus (better known as MRSA, a superbug).
“These new data reveal the true scale of antimicrobial resistance worldwide, and are a clear signal that we must act now to combat the threat,” said co-author of the study Professor Chris Murray, of the Institute for Health Metrics and Evaluation at the University of Washington.
“Previous estimates had predicted 10 million annual deaths from antimicrobial resistance by 2050, but we now know for certain that we are already far closer to that figure than we thought. We need to leverage this data to course-correct action and drive innovation if we want to stay ahead in the race against antimicrobial resistance.”








