Turning your immune system against itself: How HTLV-1 transforms immune cells into cancer
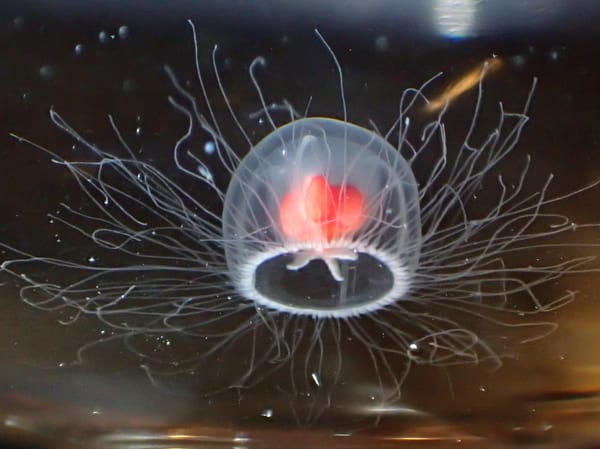
Human T-lymphotropic virus (HTLV-1) is a virus which mainly infects T cells
Human T-lymphotropic virus (HTLV-1) is a virus which mainly infects T cells, a type of white blood cell that makes up an essential part of our immune system, and induces chronic and lifelong infection. This virus spreads in the same way as HIV, via blood, sharing needles, sexual contact and breastfeeding. In the majority of people it causes no symptoms, however, in some infected individuals, infection with HTLV-1 can lead to the development of cancer. An estimated 5-10 million people are infected with HTLV-1 worldwide, for which there is currently no treatment or cure.
Now, an international team made up of scientists from Imperial College London and the Kumamoto University in Japan, have shown that the HTLV-1 is able to cause a rare type of leukemia, known as adult T-cell leukemia/lymphoma (ATL).
How does HTLV-1 cause leukemia?
The team’s research was recently published in The Journal of Clinical Investigation, and showed that HTLV infects T cells, where it inserts a copy of itself into human DNA in a process known as integration. After integration, the virus remains latent, meaning it does not multiply within the host cells or produce any viral particles. Due to this, the majority of infected individuals will not have any symptoms, and thus not know they have been infected, remaining as asymptomatic carriers throughout their life. However, 5-10% of infected individuals may go on to develop ATL, decades after initial infection.
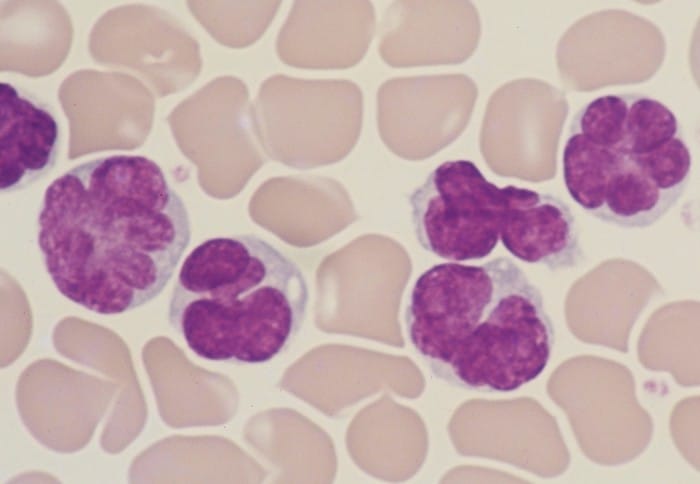
In the study, the researchers took T cells from over 87,000 healthy virus-free donors, asymptomatic carriers, and patients with ATL. Then, using bioinformatics approaches, they sequenced the RNA (a simpler, single stranded form of DNA, which carries genetic information) from these T cells, to determine how HTLV-1 causes the transformation of infected T cells into leukemic, cancerous T cells.
Under normal conditions, T cells become activated in order to fight invading pathogens. However, once their function has been completed, these immune cells need to be turned off to avoid an overactive immune response and excessive inflammation. For this reason, activated T cells will then express various proteins that stop T cell activation and restore the immune system back to normal. The team revealed that the these immunosuppressive proteins were constantly activated during HTLV-1 infection , allowing the virus to escape detection by the immune system. Overall, the system. The team believe that this persistent activation is crucial to understand how the virus triggers the development of cancer.
Next, the researchers showed that the T cells in individuals who progressed from asymptomatic carriers to cancer were over-reactive and highly activated. This led these infected T cells to over-produce proteins which keep multiplying, or proliferating. This state of overactivity is believed to make these T cells more susceptible to DNA damage, a critical factor in the development of cancer.
What is ATL?
Leukemia is a type of cancer which originates from the blood or cells of the bone marrow, and is characterised by an increased number of abnormal white blood cells. There are five major types of leukemia, one of which is ATL, for which the survival rate in adult patients falls under 50% percent. Additionally, for patients who do not respond well to treatment or relapse, this percentage drastically drops to 7% percent, signalling an essential need for novel treatment options.
What does this research mean?
Continuing this research may lead to the development of new and improved treatment options. Dr Masahiro Ono from Imperial, one of the leaders of this collaborative study, stated that “the chronic activation of T-cells could be halted by molecules that block signalling pathways that tell the cells to activate. Alternatively, treatments could target the proteins the activated T-cells create to help them proliferate.”