Novel HIV Vaccines Trialed in Humans
Three mRNA vaccines for HIV are set to complete trials in 2027
COVID is not widely considered to be a good thing. There are, however, a few good things that came out of it. Prime among these was to historic approval of mRNA vaccines, which opened up a promising scientific avenue to treat other diseases.
Problems with an HIV Vaccine
The approval of mRNA vaccines couldn’t have come too soon. Not only did the two original COVID mRNA vaccines save an estimated 1.4-4 million lives combined during the pandemic, but they are also now being trialed for diseases for which typical protein-based approaches aren’t effective, like HIV.
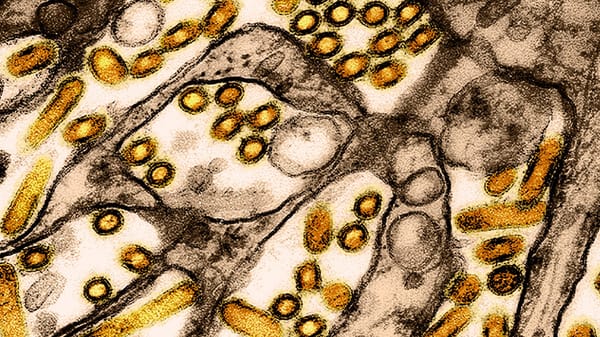
HIV is a hugely difficult virus to target using conventional vaccine strategies for several reasons. First, it is genetically diverse, meaning many slightly different versions exist and are infectious. Second, it is very good at escaping the immune system because it can mutate rapidly inside the host, meaning an effective immune response must be highly adaptable.
Vaccines designed against HIV usually try to induce production of antibodies against a protein expressed on the envelope of the cell called the Env trimer, which is the only target of neutralizing antibodies. They do this by introducing a protein that acts as a template for naïve B cells, allowing them to produce matching antibodies. This is challenging because the Env trimer binding site differs between strains and the protein has many binding sites that fail to deactivate it. Once an antibody binds to a site, it can’t bind to any others, so it is important to get the right ones. Scientists try to make the body produce broadly neutralizing antibodies (bnAbs), which attach to and deactivate many different Env protein types. Unfortunately, the body has very few naïve B cells capable of producing these antibodies, so any vaccine trying to activate them needs to be very effective and accurate.
Traditional vaccine approaches, which involve injecting different versions of the immunogenic Env sequentially, struggle to activate the B cells correctly. The Env protein on actual HIV particles has an exposed part containing many modified amino acids and a hidden, unmodified base which sits inside the shell. When the protein is simply injected into the body, it is very easy for the B cells, what few there are, to attach to the unmodified base and produce antibodies matching that part of the protein, which then cannot bind to HIV upon infection, failing to mount a defense. Protein-based vaccines are usually produced by and extracted from bacteria, so they often contain bacterial modifications, making them less accurate to the proteins they are trying to imitate.
mRNA solutions
mRNA vaccines insert small amounts of protein-coding genetic material, inducing production. When expressed on the surface of cells, the base on the Env protein is hidden from immune cells, prompting them to make the correct cure. Three mRNA vaccines have been ongoing phase 1 trial (HV302) since 2022, in a trial involving 108 participants and is expected which lasted until 2027, with participants being monitored for another two years. So far, 80% of participants who received the mRNA vaccine which produced a membrane-bound protein produced an immune response, regardless of the dose. In contrast, the non-membrane-bound version of the vaccine produced immune responses in only 4% of the participants. While we still have to wait on definitive results of this most recent clinical trial these results are promising. There is a second trial (IAVI G002) which has been ongoing since 2021 for two vaccines, but which has not posted any results.
Before any vaccine proceeds to clinical trials, it must prove safe and effective in animals. The scientists responsible for each vaccine trialed tested 5 different mRNA formulations to settle on one optimal vaccine to test. They based their determination both on the amount of bnAbs produced and on the ratio of base-binding to correctly binding ones, as well as a host of other factors, to ensure the very expensive human trials proceed only with the vaccines most likely to work.
Despite the rapid progress being made, it will likely still be several years before an HIV vaccine is widely available. Hives (with the very scary medical name ‘urticaria’) have been reported as a side effect two of the three of the vaccines currently being tested in 6.5% of participants, with effects lasting long after the trial in some cases, which will have to be mitigated before a vaccine is approved.
Progress with this epidemic is slower than it was with COVID. HIV is a tougher nut to crack for both sociological and biological reasons. 40 years after it was first recognized as a disease, only 7 people have ever been cured, while 15 million live with HIV without anti-retroviral therapy globally. Despite this bleak outlook, immense amounts of progress have been made in terms of both prevention and treatment, including long term preventative treatments and rapid treatment post-infection. With the continued effort of scientists, activists, volunteers, politicians, and the public, HIV continues to be overcome.